Dr. Philp McMillan, John McMillan
Most physicians, when pressed, would categorize measles as a respiratory illness. Ask them to elaborate, and they might mention the characteristic rash, the fever, perhaps the cough. They would be partially correct, but they would also be missing the essential architecture of the disease itself. Measles operates through deception. The virus enters through the respiratory tract, certainly, but that’s merely the opening gambit. From there, it slips into the bloodstream, travels to specific immune cells in the skin and mouth (producing the telltale rash), and only then returns to the lungs to complete its transmission cycle. To call measles purely a respiratory disease is to mistake the visible damage for the hidden mechanism.
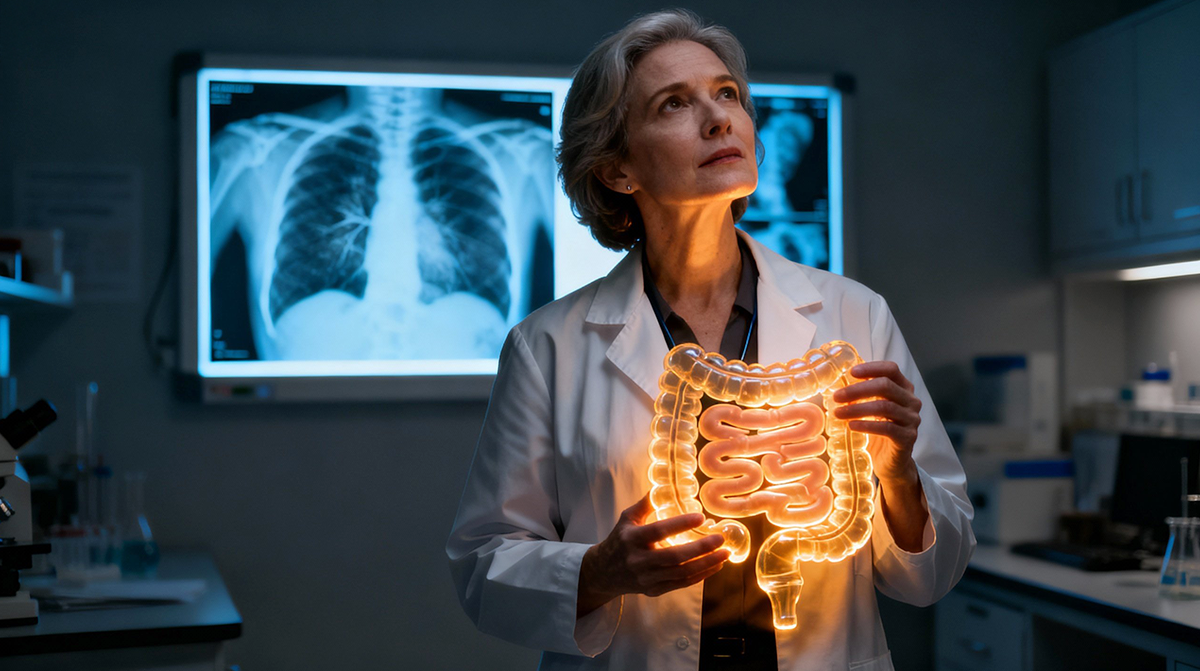
SARS-CoV-2 might be playing a similar trick. The lungs show the devastation: the ground-glass opacities on CT scans, the failing oxygen saturation, the ventilators. But emerging evidence suggests that the engine of severity, the true driver of mortality, may be hiding somewhere else entirely.
The Clue: The Mystery of MYL9
A timing paradox has occupied researchers studying severe COVID-19. Patients typically didn’t die within the first few days of infection. They deteriorated around day ten, sometimes later. Yet by that point, viral replication had largely ceased. Many patients in intensive care actually tested negative for the virus. This created a troubling clinical picture. The virus was disappearing, yet patients were dying of what appeared to be viral pneumonia. The standard arsenal of antiviral medications (Remdesivir, Paxlovid) showed modest benefit at best. They reduced symptoms and shortened hospital stays marginally, but they didn’t stop the progression to severe disease. The therapeutic window had already closed.
The smoking gun arrived in the form of a 2022 study published in PNAS. Researchers examining the micro-clots in the lungs of dying COVID patients found something peculiar: elevated levels of a protein called MYL9, or myosin light chain 9. The correlation was striking. Higher MYL9 levels predicted higher mortality with unsettling precision. The protein wasn’t just present in the lung thrombi; it appeared to be a fundamental component of the severe disease process itself.
The critical question became: Where does MYL9 primarily originate in the body?
The “Lightbulb Moment”: The Gut Connection
The answer appeared in an unrelated paper published in Frontiers in Immunology in 2021. The study had nothing to do with COVID-19. It examined myosin light chain 9’s role in inflammatory bowel disease. The findings were unambiguous. Patients with active Crohn’s disease showed significantly elevated plasma MYL9 levels compared to those in remission or healthy controls. The protein wasn’t just a bystander; it appeared to regulate the pathogenesis of intestinal inflammation itself.
The connection between these two separate observations (MYL9 in severe COVID and MYL9 in inflammatory bowel disease) suggested a provocative hypothesis. Severe COVID-19 might be fundamentally an intestinal disease. The implications require reimagining the entire disease timeline. The conventional narrative positions COVID-19 as a respiratory infection that sometimes triggers systemic complications. But the actual sequence appears to be more elaborate and more insidious.
Here’s what the revised map looks like: The virus enters through the upper airways (days 0-2), then spreads to the lungs within 48 hours. Most patients experience minimal symptoms during this phase because SARS-CoV-2 excels at suppressing interferon, the body’s first-line antiviral defense. The virus then enters the bloodstream. This is when patients might first notice a low-grade fever or mild cough. But the critical turn happens next. The virus infects the intestine, particularly the small intestine and colon, which express high levels of ACE2 receptors (the molecular doorway SARS-CoV-2 uses to enter cells). Some patients develop gastrointestinal symptoms: diarrhea, nausea, abdominal discomfort. These symptoms were often dismissed as peripheral concerns. Inside the gut, the virus replicates and triggers substantial inflammation. Over the next several days (roughly days 5-10), the inflamed intestine releases MYL9 and inflammatory cytokines into the bloodstream. These molecules travel to the lungs, where they drive the micro-clotting and cytokine storm that characterizes severe COVID-19. By the time patients arrive at the hospital gasping for air, the primary battlefield isn’t the lungs at all. It’s the gut.
Rewriting the Treatment Protocols
This framework explains several confounding patterns from the pandemic’s early days. Antivirals administered in week two of illness showed disappointing results because the critical viral replication phase had already passed. The virus had moved from the respiratory tract to the intestines, and the resulting damage was now immune-mediated rather than directly viral. Corticosteroids like dexamethasone, which suppress immune responses, showed clear benefit. This is exactly the response you’d expect if the disease was fundamentally an inflammatory process.
But the gut-centric model explains something else, something that mainstream medical analysis largely ignored: why certain disparaged treatments seemed to help. Consider vitamin D. Multiple observational studies suggested that vitamin D deficiency correlated with worse COVID outcomes. The standard explanation focused on vitamin D’s general immune-modulating effects. But vitamin D plays a specific role in maintaining the intestinal epithelial barrier and promoting microbiome diversity. If severe COVID originates from gut inflammation, vitamin D supplementation makes precise mechanistic sense.
Then there’s the treatment that became a lightning rod for controversy. Ivermectin has documented anti-inflammatory effects in the gut and impacts microbiome composition. If gut inflammation drives severe disease, a therapy targeting intestinal immune responses might work regardless of any direct antiviral activity.
Dr. Philip McMillan, a researcher and physician who has been studying COVID-19 pathophysiology, frames the broader lesson this way: “People think they understand what should happen, and they therefore try to come up with solutions based on their presumption, not based on what is actually working.” This represents a fundamental error in scientific reasoning. When anecdotal reports suggested certain treatments helped, the response shouldn’t have been dismissal based on presumed mechanisms. The response should have been curiosity. Understanding why unexpected treatments worked could reveal previously hidden aspects of the disease mechanism itself.
The Broader Implication: Assumption vs. Observation
The pandemic response was built on a framework of assumptions. COVID-19 looked like a respiratory virus, so it was treated like influenza’s more dangerous cousin. Antivirals, oxygen support, ventilation: the entire therapeutic strategy aimed at the lungs. But if the gut drives severity, medical interventions have been aimed at the wrong target. This might explain one of the pandemic’s most troubling ongoing mysteries: why excess mortality remains elevated in highly vaccinated regions. Traditional COVID deaths have declined, but overall mortality hasn’t returned to baseline. One possibility: the virus might persist as a gut infection, creating chronic low-grade inflammation that manifests not as acute respiratory failure but as cardiovascular events, strokes, or other systemic complications months after the initial infection.
Without understanding the molecular sequence (the cascade from gut inflammation to systemic disease), medicine continues to run in circles. The danger of presumption-based science becomes clear. Medical protocols were designed for a respiratory pathogen when the systemic and intestinal nature of the disease was either unknown or insufficiently appreciated. Treatments were evaluated based on their theoretical mechanisms rather than their observed effects.
The Action Plan
Severe COVID-19, in this model, is an autoimmune-like reaction driven by intestinal inflammation. The virus enters through the lungs, but it wins or loses its battle in the gut. This shifts the entire prevention and treatment paradigm. Instead of focusing exclusively on respiratory defenses, the priority becomes gut health: maintaining microbiome diversity, ensuring adequate vitamin D levels, addressing intestinal inflammation before it cascades into systemic catastrophe. As McMillan notes: “As far as I’m concerned, if you have gut problems, please don’t ignore it, fix it. It is probably the most important thing.”
Understanding the molecular steps (the precise sequence from viral entry to intestinal infection to systemic inflammation) remains the only path out of our current confusion. The alternative is to keep treating symptoms while the underlying mechanism continues its work, hidden from view, in the last place most doctors would think to look.
References:
Myosin Light Chain 9/12 Regulates the Pathogenesis of Inflammatory Bowel Disease

That’s great news!
I haven’t been invited to any of Dr. McMillian’s webinars lately. Something has gone haywire in the system I suppose.
I end up catching the YouTube videos, and some of them are weeks afterward. I never really understood how to participate by using my condition as a contributing factor. I would love to share my attempts to stay above ground with more people to get some feedback. I just can’t seem to get well.
Your article on Covid 19 possibly being a gut disease got my attention. I am not a doctor but I do recall some time ago Dr Sabine Hazan discovering that the Covid shot killed the good bugs in our body – unlike Ivermectin. Since that time I have wondered if probiotics would help to keep the gut in good condition and daily ensure I take such in the form of yoghurt and fermented foods. I hope my thinking is correct.
I have followed your articles and videos online for a number of years with interest. Carry on the good work!
Thank you, Dr Philip McMillan.