Dr. Philp McMillan, John McMillan
You trust your doctor. You trust the evening news. You trust that someone, somewhere, is paying attention to the numbers. But what if that trust is the very thing putting you at risk? Not because skepticism should slide into paranoia, but because a society that accepts narratives without cross-checking them is a society asleep at the wheel. During the pandemic, that failure had consequences. Some of them we are only now beginning to measure.
Consider the case of Cecilia Capolupo. A 46-year-old mother of two from Clapham, London, Cecilia returned from a family holiday in Devon last August feeling bloated. She and her children had indulged in pasties and fish and chips. Nothing unusual. When the bloating persisted and stomach cramps set in, she visited her GP. Probably an infection, she was told. A colonoscopy was scheduled as a precaution. On 26 September 2025, she discovered that an eight-centimetre tumour had spread to her abdominal wall, liver, and lungs. Stage four. Terminal. Two years to live.
“I came back bloated from holiday, then had stomach cramps and went to get checked out,” Cecilia told reporters. “Then I went to a routine colonoscopy and they gave me a death sentence on the same day.”
Cecilia did everything right. She was fit, she did Pilates, she went dancing with friends until the early hours. She sought medical attention promptly. And still, the cancer had already metastasised. She is not alone. Across British media in recent weeks, stories like hers have multiplied. Young, healthy adults blindsided by diagnoses that were once the province of pensioners. A 34-year-old here. A 39-year-old fitness coach there. Each case presented as an isolated tragedy, wrapped in warnings about diet and lifestyle.
The Narrative We Are Being Fed
When these stories appear, they arrive with a familiar explanatory framework. Bowel cancer rates, we are told, have increased by around 50% since the mid-1990s. The causes? Changes to the microbiome. Processed foods. Sedentary lifestyles. Family history. Each factor is plausible, and none can be dismissed outright. Ultra-processed diets and reduced physical activity do correlate with higher cancer risk. The research on this is substantial.
But here is the problem with this framing: it suggests a gradual, decades-long trajectory. A slow burn. It psychologically prepares you to accept current spikes as the inevitable continuation of something that was always happening. The implication is clear. Nothing to see here, move along.
“You are being groomed,” observed Dr. Philip McMillan, a researcher and clinician who has been tracking post-pandemic health data. “You’re being groomed into thinking that these patterns are just randomly, gradually increasing. And they are talking about it now because it’s part of the normal trajectory.”
But is it?
What the Hospital Data Actually Shows
Slow-moving lifestyle factors do not produce sudden vertical spikes. To see what is really happening, we must separate the historical trend from the post-2021 acceleration. The UK hospital admission data tells a story that the mainstream narrative conveniently obscures.
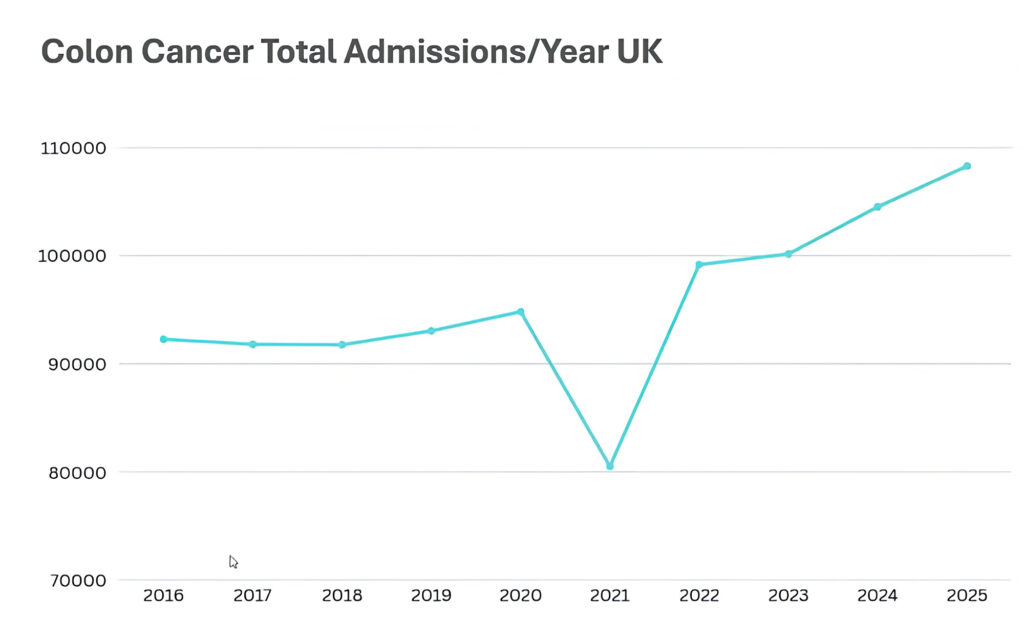
Between 2015 and 2019, bowel-related hospital admissions in the UK hovered in a stable band, between 92,000 and roughly 95,000 annually. A slight upward drift, nothing alarming. This was the old normal. Then came 2020, when admissions fell as patients avoided hospitals during lockdowns. A predictable dip. A future rebound was expected as the backlog of undiagnosed cases worked through the system.
What nobody predicted was what happened next. In 2022, admissions hit 100,000. In 2023, they climbed to 104,000. By 2024-25, they reached 108,000. The numbers did not rebound to the pre-pandemic baseline. They launched past it. The trajectory shifted from a gentle slope to something approaching vertical.
If you chart these figures, there is a visible kink in the curve. Before 2021: gradual. After 2021: steep. The pattern is even more pronounced when you examine younger age groups. Among those aged 40-49, finished consultant episodes have surged dramatically, from around 3,400 to over 5,100. The total for the 25-49 bracket has reached nearly 13,000. This is not an ageing population problem. Something else is going on.
The Question Nobody Wants to Ask
There is a factor that aligns precisely with this timeline, one that touched virtually the entire adult population in 2021 and 2022. The COVID-19 vaccines. Billions of doses were administered worldwide. In the UK, the rollout began in December 2020 and accelerated through 2021, with boosters continuing into 2022 and beyond.
When asked whether the vaccines could be driving some portion of the observed increase, health authorities respond with a familiar refrain: “There is no evidence.” But the follow-through question is crucial: what have you been looking for? At that point, the conversation typically ends. The absence of evidence is not evidence of absence. It may simply be evidence of a failure to investigate.
Several plausible biological mechanisms have been proposed. Spike protein persistence. Immune dysregulation. Interference with tumour suppression pathways. None of these has been definitively proven, but neither have they been definitively ruled out. And here is the uncomfortable truth: no good scientist would flatly deny the possibility. They would say, “We don’t know yet.” If pressed, they might add that the relevant studies simply have not been done.
What This Means for You
None of this is to say that diet and lifestyle do not matter. They clearly do. Exercise has been shown to reduce colon cancer recurrence. Inflammatory diets correlate with poorer outcomes. The mainstream advice about fibre, vegetables, and physical activity remains sound. Follow it.
But do not accept that you are simply witnessing a continuation of a decades-old trend. When you encounter news stories about rising cancer rates in younger adults, ask yourself: post-pandemic, did the trend accelerate? If yes, what is the mechanism? If you are told it is COVID infection, push further. How, specifically? And then ask the question that makes everyone uncomfortable: is it possible that this could be connected to the mass vaccination campaign?
“There is a responsibility now to ask hard questions, challenge your trusting people, force them to think, not just accept what is in front of them,” Dr. McMillan noted. “Because as you can tell, whatever you watch, whatever you read, there is usually an agenda behind it. You have to become wiser and better prepared for the future.”
Cecilia Capolupo rushed to her GP at the first symptom. It was already too late. If the UK had implemented screening at 45, as Australia has, she might have had a fighting chance. The 2026 data, when it arrives, will likely show the curve continuing its steep ascent. By then, the question will no longer be whether something changed in 2021, but why we waited so long to ask.

0 Comments