Dr. Philip McMillan, John McMillan
Here is something most people never think about: your body is full of viruses that never left. If you had chickenpox as a kid, the varicella zoster virus is still inside you, tucked away in the nerve roots along your spine. If you ever caught mono from Epstein-Barr virus, it is still there too, sitting inside your B cells. Herpes simplex? Parked in a nerve behind your cheekbone. These are not active infections. They are old tenants who moved in years ago and never moved out. Your immune system knows they are there and keeps them in line. For most of your life, that arrangement works just fine.
The question is: what happens when the thing keeping them quiet is thrown off balance?
A recent hypothesis paper on the potential impact of SARS-CoV-2 spike protein on HIV reservoirs has started to answer that. Clinician and researcher Dr. Philip McMillan has explored the paper in detail, laying out how spike protein, whether from infection or vaccination, can wake up viruses that have been dormant for decades.
The Hostage Situation
To understand why this matters, it helps to understand what “dormant” actually means at the cellular level. HIV is the clearest example. It is a retrovirus that rewrites its genetic code into your DNA. It literally becomes part of you. Even with treatment, the virus is never truly gone, just kept quiet. As Dr. McMillan put it: “An inefficient virus kills its host. A clever virus stays with it.”
Other viruses play the same game in different hiding spots. Varicella zoster buries itself in nerve cells. The immune system parks T cells around the infected neuron like guards outside a locked room. They cannot destroy the cell because neurons do not grow back, so instead they stand watch. Dr. McMillan describes this as a biological hostage crisis: “They can’t afford to kill him because he knows information and he may have some way that he does damage if he dies. And so the immune system has got him locked in a room, doesn’t let him get out, but can’t kill him and can’t blow up the house.”
EBV in B cells, herpes simplex in cranial nerves, cytomegalovirus in various tissues: the same standoff plays out across the body. The trouble starts when the guards get overwhelmed.
How Spike Protein Picks the Lock
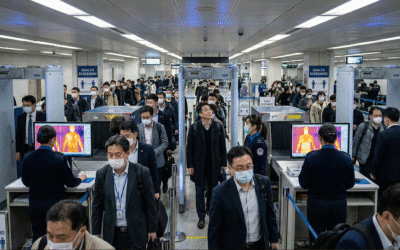
What makes SARS-CoV-2 spike protein different from, say, influenza is how far it travels. Flu largely stays in the lungs. Spike protein does not. Once it enters the bloodstream, it binds to tissue throughout the body: heart, kidneys, blood vessels, brain, even the skull membranes. A separate paper on spike protein persistence in meningeal tissue shows how widely it spreads and how long it lingers.
The HIV reservoir paper describes two pathways to reactivation. In the first, a bystander effect, spike protein enters an uninfected cell via a lipid nanoparticle or viral particle. That cell produces spike protein, kicks off inflammatory signaling, and releases cytokines that drift to a neighboring cell harboring a sleeping virus, flipping a switch on the dormant genome. The virus wakes up not because it was directly attacked, but because of what happened next door. In the second pathway, spike protein production happens inside a cell already containing latent virus, destabilizing the dormant DNA from within.
Dr. McMillan stresses that reactivation is not a coin toss. It requires five things happening at once: immune activation, systemic cytokine spillover, persistent immune activation, T-cell dysfunction, and exposure to cells carrying dormant virus. Knock out any one, and the chain breaks.
So where does the greater risk sit: vaccination or infection? Both carry latency risk through slightly different mechanisms. Vaccination triggers significant cytokine release without viral replication. Infection brings both. Neither is risk-free. And because vaccination does not prevent reinfection, cumulative spike protein exposure keeps climbing. A 2022 German study on varicella zoster reactivation found nearly double the risk of shingles in vaccinated individuals compared to unvaccinated. That finding deserves close attention, even as the broader picture continues to develop.
Not Sick, but Overloaded
Here is the part that might surprise people: the individuals most at risk are often not the ones you would expect. They are not walking around with obvious immune deficiency. They are high-functioning people who have been pushing through low-grade symptoms for years, operating close to what Dr. McMillan calls their “recovery limit.”
Many already have three of the five cascade steps ticking along in the background: dormant virus (nearly universal), mild T-cell dysfunction, and low-grade immune activation. One more immune trigger supplies the final two steps and completes the set.
The pattern is hard to miss once you know it. A history of chickenpox, recurring cold sores, allergic tendencies, aches that flare with stress. Migraines, tingling in the hands or feet, brain fog, broken sleep. These people have been told repeatedly that their blood work looks fine, which leads to frustration and a tendency to just power through. And powering through makes things worse.
Fatigue, in this light, is not a personal failing. It is the body pulling the emergency brake, forcing rest so the immune system can work without competing for energy. Ignore that signal and you burn through your recovery reserves, opening the door to the very reactivation you cannot afford.
The Quiet Protocol
When people feel immunologically fragile, the instinct is to boost. Take more supplements. Crank up the immune system. Dr. McMillan argues this is exactly the wrong move. A revved-up immune system does not protect against reactivation; it fuels the dysregulation that causes it. The goal is balance: quiet the immune noise, protect recovery capacity, stop piling stressors on top of each other.
The foundations do not require a prescription. Sleep is the single most important immune regulator, preserving the CD8 T cells whose job is to keep latent viruses in check. Blood sugar stability matters more than most realize: insulin spikes create inflammatory noise, exactly what destabilizes latency. Slow-release foods like yam, cassava, and cornmeal beat anything that floods the system with glucose at once. Stress pacing, deliberately not stacking obligations when symptomatic, reduces the cortisol surges that throw immune responses off target.
When it comes to supplements, the list is short. Magnesium stabilizes neuroimmune signaling and supports T-cell and mitochondrial function. A lot of people are deficient and have no idea. In hospitals, intravenous magnesium is given before other drugs for dangerous heart rhythms and in preeclampsia: that is how powerful its calming effect is. Vitamin D supports immune tolerance rather than stimulation, but too much can actually heighten immune activation, so cycling on and off beats chasing high numbers. Omega-3 fatty acids lower baseline inflammation without suppression, supplying raw materials for specialized molecules (resolvins, protectins, maresins) that actively wind down inflammatory responses. Dr. McMillan has personal skin in this game: severe childhood eczema that disappeared entirely once he began taking omega-3s, proof that individual inflammatory thresholds sometimes need specific support.
The common thread is moderation. Supplement in cycles, not continuously. Eat in ways that avoid metabolic spikes. Rest when your body tells you to. In an era of repeated spike protein exposure, protecting your recovery capacity may be the single best defense against the ghosts of viruses past.
The clever virus waits. Our job is to make sure the guards never leave their post.


Please keep me informed of the stages of all virus passed and present thank you
Thank you Philip for your articles. Valuable . . . .and we should all remember: The way is the goal ! Learning, understanding helps us to play the game. MDs are at maximum (!) good coaches (most of them – 80% and up!) are not. They stand on the sidelines at the soccerfield – but you have the ball and you – only you – can play the game – not they. Therefore you must train, learn all these things down to your bone . . . . To win the game, to shoot the goal(s).
Dr. McMillan, thank you for taking the time to explore this area with depth and intellectual courage. The discussion around viral latency, immune balance, and long-term biological consequences deserves careful, methodical investigation — especially when it challenges us to look beyond surface-level explanations.
True scientific medicine advances not by defending prior assumptions, but by asking better questions and following the data wherever it leads. The mechanisms you’ve outlined — particularly around immune regulation, persistence, and reactivation thresholds — highlight how much complexity remains to be understood.
What I appreciate most is the emphasis on due diligence: not alarmism, not dismissal, but deeper inquiry. If there are areas mainstream research has not yet fully examined, that is not an indictment — it is an invitation for further work.
Progress in medicine has always depended on those willing to explore the edges carefully and responsibly. Encouraging robust, transparent, and independent investigation into viral latency and immune dynamics can only strengthen the field and public trust.
Thank you for contributing to that process.